The U.S. has one of the highest levels of monkeypox in the world, according to new data from the Centers for Disease Control and Prevention (CDC).
As of Tuesday, July 26, the U.S. had a total of 3,591 confirmed and reported monkeypox cases, according to federal and global data, just behind the world’s highest country total in Spain, which was 3,738 on that date.
Monkeypox is endemic to Africa, but began spreading outside the continent in May, with the first cases showing up in Spain and Portugal, then appearing in the U.K. and Germany.
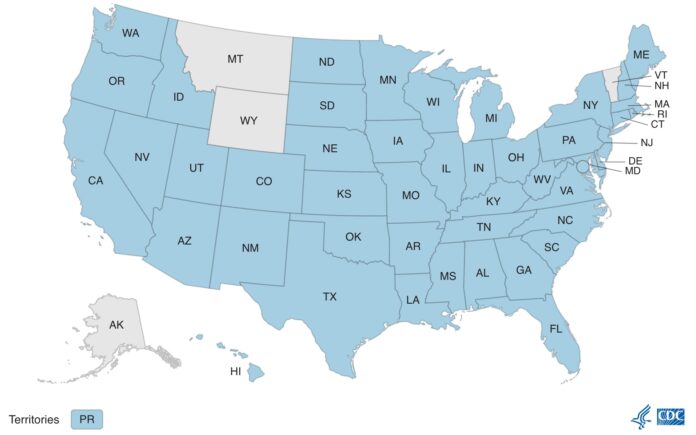
The CDC data show monkeypox cases in 46 states plus the District of Columbia and Puerto Rico. Only Alaska, Montana, Vermont and Wyoming have yet to report cases. The highest number of cases is in New York, with 1,092 cases, followed by California, Illinois, Georgia, Florida and D.C. Pennsylvania and New Jersey are in the next tier of cases with close to 100 each. Delaware also has reported a few cases.
As PGN has been reporting since May, infectious disease experts have warned that the number of monkeypox cases is probably significantly higher than the numbers being reported, and more testing and contact tracing would reveal a far larger number of cases.
“I think they’re going to be reluctant to use the word pandemic, because it implies that they’ve failed to contain this, and I think at this point we’ve failed to contain this,” Dr. Scott Gottlieb told CBS “Face the Nation” on July 17. Gottlieb was Food and Drug Administration (FDA) commissioner under President Obama.
Gottlieb said the official U.S. total of confirmed cases is only a small fraction of the cases in the country.
The World Health Organization (WHO) declared the outbreak a Public Health Emergency of International Concern on July 23 following a meeting that day of the International Health Regulations Emergency Committee (EC). That declaration is the strongest call to action the agency can make. The most recent such announcement was for COVID-19 in 2020. Such a declaration signals a global pandemic. WHO has been contemplating the declaration for several weeks as cases surged.
The WHO announcement came a month after the agency decided on June 25 that the severity of the disease spread did not warrant a global emergency declaration at the time. But now the outbreak is in twice as many countries as it was in June, with 19,188 monkeypox cases reported in at least 76 countries, primarily transmitted among men who have sex with men.
Dr. Tedros Adhanom Ghebreyesus, the WHO’s director general, overruled the committee, which was unable to reach a consensus about the severity of the outbreak, by declaring the monkeypox threat.
The WHO declaration means the risk of the disease spread requires a coordinated international response.
In a statement, Ghebreyesus said that although the “risk remains low for the time being,” monkeypox presents “a clear risk of further international spread.” On July 27, the Associated Press reported that Ghebreyesus “advises men at risk of monkeypox to consider limiting sexual partners for now.”
The U.S. has yet to declare a public health emergency, despite the surge in cases in recent weeks. On June 28 the CDC announced it was activating its Emergency Operations Center (EOC) in response to the spreading monkeypox outbreak in the U.S. At that time the CDC said that the activation of EOC “allows the agency to further increase operational support for the response to meet the outbreak’s evolving challenges.”
In a press briefing on July 26, White House COVID-19 Coordinator Dr. Ashish Jha said, “The international community must work together to protect individuals that have been impacted by monkeypox, and those most at risk of contracting the virus.”
The White House has yet to appoint a monkeypox coordinator, despite President Biden voicing concerns about the disease back in May.
During a press briefing earlier this month, CDC Director Dr. Rochelle Walensky said, “We anticipate an increase in cases in the coming weeks. We know monkeypox symptoms usually start within three weeks of exposure to the virus, so we anticipate we may see an increase in cases throughout the month of July and into August.”
Jha said Tuesday that “We want to make sure that all Americans understand that we have taken, we continue to take, this virus seriously.”
But it was revealed the day before Jha’s statements that the U.S. failed to deliver much-needed vaccines to contain the spread of monkeypox. Instead, as the New York Times broke the story, 300,000 vaccine doses sat in a facility in Denmark, unused and undelivered while lack of coordination of the CDC efforts on monkeypox failed to have those vaccines sent stateside.
In June, the CDC had announced the National Monkeypox Vaccine Strategy (NMVS). The NMVS was supposed to expand availability of monkeypox vaccine to try and control the widening outbreak of the disease that is endemic to Africa and has not had a U.S. outbreak since 2003.
The White House fact sheet on monkeypox vaccines states that in addition to offering vaccines to those who have had known exposure to the virus, federal health officials would make vaccine available to men who have sex with men who have had multiple recent partners in venues where it is known monkeypox virus was spreading or in a geographic area where monkeypox is transmitting.
That has not happened. In New York City, Mayor Adams confronted HHS officials over the failure to provide enough vaccine. In a statement July 13, Adams said he and his health commissioner, Dr. Ashwin Vasan, pleaded for more help in the call with Health and Human Services Secretary Xavier Becerra and CDC Director Rochelle Walensky. Infections in New York City make up nearly a third of the national case count.
“The U.S. government intentionally de-prioritized gay men’s health in the midst of an out-of-control outbreak because of a potential bioterrorist threat that does not currently exist,” James Krellenstein, a Brooklyn-based gay health activist, told the New York Times. Krellenstein had been urging health officials to make the vaccine more widely available since June.
Gary Disbrow, who oversees the vaccine for the U.S., told media that the Biden administration was “moving very quickly because we take this very seriously.”
“We thought it prudent to get as many doses as we had available over here, fully understanding that if the doses are not used there would be a potential impact on smallpox,” he added. “We moved very quickly based on the number of cases we saw.”
There have been no smallpox cases in the U.S. since 1949. In 1980, the World Health Assembly declared smallpox eradicated (eliminated), and no cases of naturally occurring smallpox have happened since.
In Philadelphia, the vaccine is available through the health department by invitation only.
The majority of cases reported in the U.S. have been related to male-to-male sexual contact, according to the WHO. But last week, federal officials confirmed that two children in the U.S. had tested positive for monkeypox, one in a toddler and another an infant. Both cases were in California.
Health officials in the U.S. and elsewhere have stressed that although monkeypox is affecting the “gay, bisexual, and other men who have sex with men” communities most significantly, the virus can affect anyone who has close contact with people who have monkeypox, including children.
In his opening statement declaring the emergency, the WHO director noted that “Person-to-person transmission is ongoing and is likely underestimated,” and said “In Nigeria, the proportion of women affected is much higher than elsewhere, and it is critical to better understand how the disease is spreading there.”
Cases among women have not been highlighted by the CDC in the U.S.
More information on monkeypox symptoms and treatments is available at cdc.gov and the WHO Director-General’s statement is available at who.int/.
