I recently was making the hour-long trek back from Nemours Children’s Hospital in Delaware, and I was feeling great! Avery finally had a good day: She was less swollen than she’s typically been and starting to look like an actual baby. I had a delicious lunch and got some work done at the hospital, and I was jamming out to “Phantom of the Opera” cruising down I-95 with no traffic.
As I finished belting out the last verse of “Music of the Night,” I thought back to some of my other drives to and from the hospital — the distractions not coming from the music but from my hysterical crying or the endless questions and anxieties whirring through my brain. I’m glad things have settled down into this new, normal routine, I thought to myself.
But just as quickly as I thought it, my brain smacked me back: This should not be normal!
I replayed my seemingly good day with more cynical eyes: I hit the road a few minutes later than I had intended to because Avery had pulled her nasal cannula prongs out of her nose and I awkwardly was walking back and forth to her door waiting for a nurse because I was too afraid to try to push them back in myself. While holding her, she gave a little cough that sent her monitors into beeping overdrive and put my own breathing on edge until a nurse checked on her and assured me her breathing was just “drifting” again but she had fixed herself. I spent a while bent over Avery’s isolette saying goodbye — making sure to give her the schedule of which days Ashlee and I would be there to see her in the next week and hesitantly pulling my finger out of her grasp to collect her bag of laundry that I had to bring home and wash.

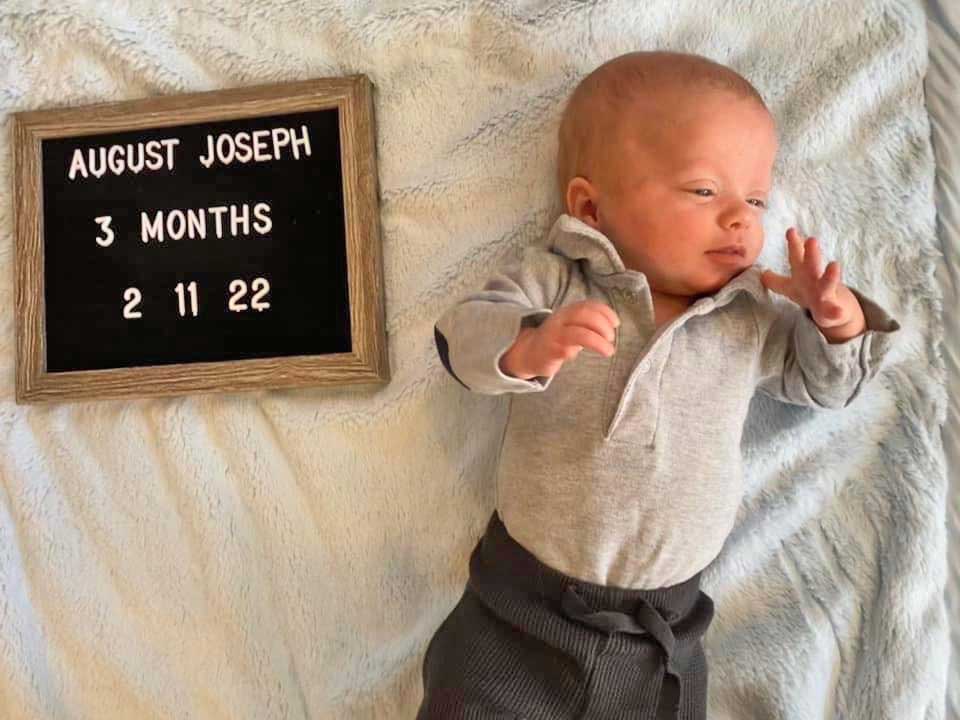
None of that is normal, I reminded myself. Avery is 3 months old now and should be dazzling us with her first laughs, keeping us up all night, growing into chubby cheeks, starring in a million social media posts, learning tummy time and experiencing so many other normal aspects of being a baby. But, that reality is based on the presumption that being a baby means being healthy and being cared for by your parents — neither of which are part of her, and our, experiences. The NICU carries with it a lot of trauma. For the babies, it’s the separation from their loved ones, the substitution of machines and boxes for caring hands, the needles and tests and physical pain. And for parents, it’s the ache of being helpless to stop your child’s pain while always waiting for The Phone Call that could bring dreaded news.
But with any ongoing trauma, after a while you get desensitized to the other-worldliness of it — your mind’s way of helping you manage a situation that you just have no mental or emotional framework for, I guess.
I encountered this many times during my reporting at PGN, first as a staff writer and later as editor. I remembered interviewing so many people about their experiences during the height of the HIV/AIDS epidemic in the 1980s and ’90s who told me matter-of-factly about the literal dozens of friends they had lost. Dozens?!, I remember thinking time and time again. And yet they were able to share so calmly. I talked to many parents and friends of community members lost to violence, checking in with them on the yearly anniversaries, and every year was struck by how collected they were when reflecting on what were likely some of the worst days of their lives.
While we’re more than fortunate, and much more fortunate than many, to have two babies who’ve made it this far, I can see from this side of trauma that it’s not that these people I had interviewed necessarily found the secret ingredient to dealing with pain or grief or anxiety — rather, they likely had to learn to live with it by normalizing a situation that was nowhere near normal. It’s a coping strategy that can help you adapt to ongoing trauma but it does make you lose perspective of the gravity of what you’re going through. Sooner or later, though, trauma finds its way of sneaking through the cracks in whatever facade of normalcy you try to construct.
One of my recent wake-up calls was while reading “Juniper: The Girl Who Was Born Too Soon” (a must-read for any NICU parent and a should-read for all else!). The memoir is by a pair of married journalists whose daughter was born at 23 weeks, weighing 1 pound, 4 ounces, slightly more than Avery. The book details Juniper’s NICU experience, which held many similarities to Avery’s — the size, the translucent skin, the near-fatal intestinal perforations. It spares no expense when it comes to graphic details, describing to a T the unpleasant feast for the senses that is the NICU, which transported me right from my couch into the hospital on our worst days.
But what resonated the most was the authors’ understanding of the NICU’s visceral attack on the very core of what it means to be a parent. “You can’t parent a baby in a box,” they write. Seeing it that simplified, from someone else’s eyes, really drove home that trying to normalize the situation was just futile.
But, coping with any ongoing trauma does require a fine balancing act between accepting and refusing to accept the situation as your reality. In our case, I have to distance myself somewhat from the anxiety of having a long-term NICU baby because I can’t be changing August’s diaper or making crafts with Jackson while a teary-eyed mess. Yet, the worry and overwhelm is never far.
So, what is a stressed-out parent to do? Here are a few things we’ve found helpful to surviving the NICU, which may also have some applicability for other types of trauma.
Seek out stories and support: The NICU is an extremely isolating environment. Each family there is dealing with their own issues and, even physically, parents are laser-focused on their individual baby, rarely interacting with one another when going to and from their bedside. And, like us, few people have any direct experience with, or inkling of what the NICU is really like before you get there; while you appreciate those well-meaning folks in your life offering support, their disconnect from the situation is palpable.
So, we sought out new connections with those who have been there. We joined several Facebook groups for Philly-area NICU parents, IUGR parents, and more, and even though we’ve been relatively silent in those groups, it’s heartening to see other parents rattling off oxygen saturation rates or to whom we don’t have to explain the difference between a preemie’s gestational, actual and adjusted ages. We’ve met several fellow NICU parents at our babies’ hospitals that we keep in touch with, and we’ve also come to see the nurses as our allies. Sharing caregiving duties for your babies with total strangers was a weird dynamic to adjust to, but we ultimately realized they not only know our babies well, but they know the NICU in and out, and they can offer not just medical advice for the babies but significant emotional support for us as well.
Let yourself feel: Whenever anyone is in a crisis situation, it seems to be customary for others to try to cheer them up by commenting on how “strong” they are; we’ve heard this countless times once the babies’ complications started snowballing. Sure, there’s truth to taking strength to weather a challenge, but that well-intentioned observation also presupposes that the person isn’t struggling, or that they’re choosing to valianty forge on instead of just surviving because they have to. Sometimes in the last few months, I didn’t want to feel strong; I wanted to cry and rage and smash breakable things and ignore all of my responsibilities and drown myself in chocolate and red wine. But the expectation that you have the capacity to be “strong” in such low points attaches an element of shame to letting yourself truly feel when you’re in pain. Especially for parents of kids dealing with medical issues, there’s added pressure to put up a brave front, but I think it can show just as much strength to let yourself feel, and express, the depth of the emotions you’re feeling. And if that means breaking plates and gorging yourself on Godiva and Cabernet, so be it.
Acknowledge that life is changed: Initially, I was aghast that the world didn’t stop when the babies were born: Bills continued to come due, my car needed an oil change, Jackson needed gifts for his preschool friends’ birthday parties. Our little world seemed upside-down, so it felt like the rest of the world should follow suit.
Realistically though, we had to hop back on that merry-go-round, even though we already felt changed by the NICU — more worried, more cautious but also more appreciative and more humbled. We had to adjust our lives to those new realities. We’ve had to learn how to not get bogged down by the constant anxiety, to welcome and even invite help, to feel confident being our babies’ advocates even when we don’t at all feel confident as their parents yet.
Importantly, we’ve had to adapt to seeing both the bad and the good in our lives simultaneously, but not singularly. The NICU is an all-encompassing experience, and it’s very easy to view the world solely through the lens of that trauma. However, that would cloud out all the good that has happened right alongside the bad: all of the odds the babies have beaten, the way Jackson has blossomed as a big brother, the constant support we’ve felt. Giving yourself leeway to appreciate and even enjoy those good parts of life without guilt, even if it’s just having an awesome “Phantom of the Opera” jam session without feeling bad you’re driving away from your baby, doesn’t diminish the pain of the bad days. But it does at least help you remember what “normal” feels like.
