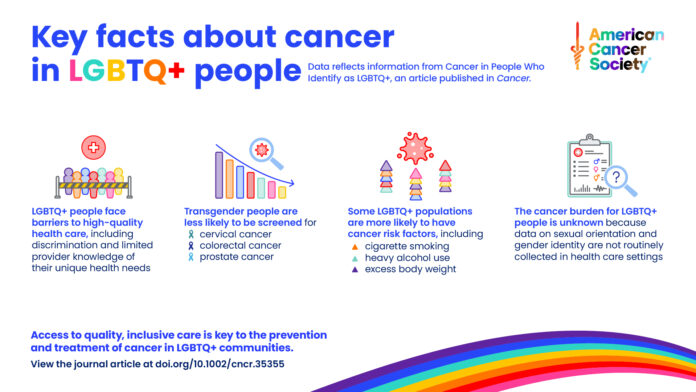
The American Cancer Society (ACS) has released a groundbreaking new study, “Cancer in People who Identify as Lesbian, Gay, Bisexual, Transgender, Queer or Gender-nonconforming (LGBTQ+)” to coincide with the start of Pride month in June. The data in the report delves into every aspect of cancer care and treatment and reveals that at every point, LGBTQ+ people were discriminated against and found access to care difficult if not insurmountable. The study also revealed that LGBTQ+ people had elevated risk factors for cancer, particularly in breast, cervical, prostate and colorectal cancers, and that in turn led to more cancer while other factors keep queer and trans people from accessing care.
The report—which has gone unremarked in mainstream media with not a single newspaper or online news service reporting this data—reveals the latest statistics on the prevalence of cancer screening and modifiable risk factors in LGBTQ+ people. More than 40% of all cancers in the general population are attributable to potentially modifiable risk factors, such as tobacco use, excess body weight, alcohol consumption and unhealthy diet—these were all higher in LGBTQ+ people.
There is also a review of literature on cancer occurrence and obstacles to cancer prevention and treatment for those same LGBTQ+ groups. These new and comprehensive findings are published in the medical journal “Cancer” and also in what ACS calls a “consumer-friendly” journal, “Cancer Facts & Figures 2024 Special Section: Cancer in People Who Identify as LGBTQ+.” The 18-page report has a plethora of details for LGBTQ+ people, but the key finding is that stress and discrimination are defining factors in how lesbian, gay, bisexual, transgender, queer and gender-nonconforming people access cancer care and that disparity is leading to far worse outcomes at every level.
ACS says that the greatest health disparity faced by LGBTQ+ communities is the “presumption-of-care gap,” by which they mean the fear that a provider will refuse care due to gender identity or sexual orientation. ACS says that rather than being a misperception for LGBTQ+ patients, the concern is “especially valid for the 20% of this population who reside in the nine states where it is legal to refuse care to LGBTQ+ individuals due to ‘conscience clauses’ that allow healthcare providers, staff and insurers to deny care and services based on personal and religious beliefs.”
Rebecca Siegel, senior scientific director, cancer surveillance at the American Cancer Society and senior author of the study said in a statement, “One of the biggest take-aways from our report is that LGBTQ+ people are probably at higher risk for cancer, yet experience multiple barriers to high-quality healthcare access like discrimination and shortfalls in provider knowledge of their unique medical needs.”
Siegel said, “Everyone deserves an equal opportunity to prevent and detect cancer early, which is why it’s so important to remove these roadblocks for this population.”
ACS reports LGBTQ+ individuals in the U.S. have elevated prevalence of smoking, excess body weight and other factors that increase cancer risk. For example, ACS states bisexual women are twice as likely as heterosexual women to smoke cigarettes (23% versus 10%) and drink heavily (14% versus 6%).
Similar findings were uncovered in another new and groundbreaking study conducted by researchers at Harvard T.H. Chan School of Public Health, the University of Utah, Boston Children’s Hospital and Columbia University. That study found that sexual minority women—those who identify as bisexual or lesbian—die earlier compared to heterosexual women. Those data were reported in the journal JAMA (The Journal of the American Medical Association), a peer-reviewed medical journal published 48 times a year by the American Medical Association. It publishes original research, reviews and editorials covering all aspects of biomedicine.
The key finding is that compared to heterosexual women, bisexual women died 37% sooner and lesbian women 20% sooner than their heterosexual peers.
The ACS study states that “minority stress” is a likely contributor to behaviors like smoking that increase cancer risk as is revealed in other studies. ACS says that although these findings suggest cancer disparities, cancer incidence and mortality for this population are not available because sexual orientation and gender identity are not routinely collected in healthcare settings, despite the community’s willingness to report this information. That fact in itself is discriminatory and leads to worse health outcomes for LGBTQ+ people.
But the ACS report found that discrimination is at every point in the healthcare journey and even includes GNC lesbians and trans persons having conflicts with bathroom access in healthcare settings. ACS says that more than half of LGBTQ+ adults have experienced harassment, including slurs, microaggressions, sexual harassment, and violence, and 1 in 3 have experienced discrimination simply trying to use the bathroom. ACS says that this discrimination is most common among people of color and extends to health care settings. One in 6 LGBTQ+ adults, and 1 in 5 transgender adults specifically, avoid health care due to previous discrimination.
Similarly, LGBTQ+ individuals with cancer experience disparate outcomes across the cancer continuum, says ACS, including prevention, screening and early detection, diagnosis, treatment and palliative care. ACS says, “Although knowledge of these inequalities is accumulating, surveillance data on cancer in the LGBTQ+ population are currently limited to national surveys on risk factors and screening. Population-based data are unavailable for incidence and mortality because sexual orientation and gender identity are not consistently collected in medical records.”
ACS explained how the National LGBT Cancer Network estimates that there are one million LGBTQ+ cancer survivors in the U.S. But compared to the general public, LGBTQ+ cancer survivors are more likely to have poor physical and mental health, have higher prevalence of cigarette smoking and heavy alcohol use and frequently experience homophobia and discomfort expressed by health care providers. Transgender patients also face discrimination in palliative care, including deliberately discourteous treatment, refusal to acknowledge gender identity or use preferred name, and privacy violations.
ACS says these circumstances and experiences reduce quality of life for cancer survivors, especially for those with high minority stress and/or low social support. For example, LGBTQ+ individuals with cancer are 3 to 6 times more likely to report high or very high distress levels.
“We are very proud of this report,” said Tyler Kratzer, associate scientist II, cancer surveillance research at the American Cancer Society and lead author of the study. “It is meant to facilitate critical conversations around the need to improve the routine collection of sexual orientation and gender identity data at all levels of healthcare.”
For example, ACS found “provider perceptions are not in alignment with patient preferences; 80% of clinicians in a national study believed their patients would refuse to disclose their data, while only 10% of patients reported such refusal. In fact, LGBTQ+ patients are most likely to understand the value of this information, suggesting that lacking data collection can be largely solved by provider education.”
For the study, researchers examined the prevalence of risk factors across the U.S. based on the National Health Interview Survey (for information on sexual orientation) and the Behavioral Risk Factor Surveillance System (for gender identity), which are both collected by the Centers for Disease Control and Prevention (CDC).
Other highlights from the report include:
Excess body weight appears to be elevated among bisexual women according to one national survey, although the gold-standard source for this metric that includes an in-person physical exam—the National Health and Nutrition Examination Survey—does not collect data on sexual orientation or gender identity.
The prevalence of cancer-causing infections, such as human immunodeficiency virus (HIV), human papillomavirus (HPV), and hepatitis C virus (HCV) are considerably higher in some LGBTQ+ population groups. According to the CDC, for example, 70% of HIV infections are attributed to male-to-male sexual contact (versus 22% to heterosexual contact and 7% to injection drug use). HIV-infected individuals are at a higher risk for at least 10 cancers.
Screening for some cancers is low among transgender people; for example, only 46% of transgender men are up-to-date on colorectal cancer screening compared to 60% of cisgender men and 68% of transgender men with a cervix are current for cervical cancer screening compared to 87% of cisgender women.
Another key finding in the report is that only 25% of medical students are confident in knowing what the healthcare needs of transgender patients are while 30% are not comfortable treating transgender patients, according to one study.
ACS states that “Insufficient access to high-quality care, limited provider knowledge of LGBTQ+ patient needs, discrimination in the health care setting, and a lack of population-based cancer occurrence data are all barriers to health equity that need to be addressed.”
The report cites a list of what the ACS is doing to address cancer disparities in LGBTQ+ communities in advocacy and outreach. It also provides resources for LGBTQ+ individuals with cancer and their families.
“All people should have a fair and just opportunity to live a longer, healthier life free from cancer,” said Lisa A. Lacasse, president of ACS’ advocacy affiliate, the American Cancer Society Cancer Action Network (ACS CAN) in a statement. “As part of our mission to advocate for public policies that reduce the cancer burden for everyone, ACS CAN urges policymakers and lawmakers to prioritize policies that address the serious challenges and barriers to comprehensive access to health care that LGBTQ+ people experience. Importantly, passing laws that facilitate and increase the appropriate collection of sexual orientation and gender identity data is crucial to better understanding cancer disparities and to ultimately improving health outcomes.”
The American Cancer Society is a leading cancer-fighting organization committed to ensuring everyone has an opportunity to prevent, detect, treat and survive cancer. For more information, visit cancer.org or call ACS’s 24/7 helpline at 1-800-227-2345.