Part two in a three part series. Some names have been altered to protect privacy.*
“So many of us never thought we’d live to see 40. We never planned for 80.” At 73, Sam Miller* works for a graphic design company in New Jersey. He’s been living with HIV for some years and considers himself “blessed” to have survived the epidemic that took many of his friends when he was younger.
“I actually got HIV later in life,” Miller says. “No one thinks about getting HIV at 60, but you’re never too old to make mistakes. I was so vigilant about safe sex when AIDS was everywhere. I was that guy handing out condoms in the bars like party favors.”
Then, Miller says, at 60 he fell in love with a younger man after the breakup of a long-time relationship. “I broke all my own rules that had kept me safe for years,” he laments. “We didn’t get tested, we didn’t practice safe sex, and he was positive and didn’t know it.”
Miller says being HIV+ means “retirement is a ways off. These drugs don’t pay for themselves.” Miller says he needs the healthcare plan at his job to “support my drug habit,” which includes Biktarvy, which costs about $90k a year without insurance.
For Miller, his job and his health are now inextricably linked. “I am otherwise pretty healthy,” he says of his HIV status. “So I think if these meds continue to work for me, I have another 10 years, maybe more. But only if the drugs can be paid for by insurance. Otherwise, I just don’t know.”
Miller says there’s “some stress involved” in having to keep working into his 70s, and he feels that there could be pressure on him to retire from the company itself in the next few years. “No one knows my HIV status except close friends and anyone I have sex with. So I hope I never have to tell my employer: ‘please don’t force me to retire as it could kill me.’”
HIV can be a complicating factor for many older gay, bisexual, and trans people. Many elders like Miller find that they have “fallen out of the habit of safe sex” after having been in long-term relationships that were monogamous. Others say that no attention is paid to the issue of HIV positivity and queer and trans elders.
“We don’t talk about HIV much anymore,” said Cerise, a trans woman living in Nicetown. “But it’s an issue for a lot of us. It’s an issue for everyone I know.”
At 63, Cerise doesn’t consider herself old “by any stretch,” but says that the HIV+ status of many of her trans friends has created financial hardship for them and “makes it hard to make a living, you know?”
Cerise, who asked that we not use her last name “because you never know, people can be scary,” said that while she had “escaped” being HIV+, “there are many trans girls out there dealing with it and finding it plenty hard to get those meds.” She wonders if that will impact their life expectancy.
For Cerise, there is another medical complication: diabetes. “My whole family has it,” she says. “I have seen the whole thing — losing toes, losing their vision. It’s a bad disease and it’s hard to maintain. I find it very hard to maintain.”
Cerise said she sees her doctor “as regular as I can,” but that “it’s all about having enough money for things.” Cerise does hair out of her apartment and says her income is not as dependable as she would like.
Diabetes impacts 1 in 9 Americans, and Black Americans are disproportionately affected by the disease, being almost twice as likely as white people to develop type 2 diabetes by middle age. In addition, those who get diabetes are significantly more likely to suffer complications such as blindness, kidney disease and amputations than their white counterparts — something Cerise witnessed in her family.
“Insulin costs a lot,” Cerise said, explaining that you have to have Medicare or Medicaid to afford it. “And you can’t always get that because they don’t make it easy to qualify. It’s not as simple as people think.”
Cerise said there are other health issues that older trans women face, like maintaining hormone treatments and getting prophylactic screenings for cancer.
LGBT people have lower rates of health insurance coverage than the general population, which is a result of higher costs and outright exclusions from insurance plans. According to a recent study conducted by the health insurance website HealthCare.com, 1 in 8 LGBT+ Americans face health insurance discrimination, with respondents saying they have experienced discrimination from their health insurance provider.
A 2020 study by the Center for American Progress (CAP) found that “many LGBTQ people continue to face discrimination in their personal lives, in the workplace and the public sphere, and in their access to critical health care. This experience of discrimination leads to many adverse consequences for their financial, mental, and physical well-being. Many LGBTQ people report altering their lives to avoid this discrimination and the trauma associated with unequal treatment.”
CAP found that the pandemic exacerbated these issues for LGBT elders and that exclusion from health care plans belonging to partners was an issue that many LGBT people face.
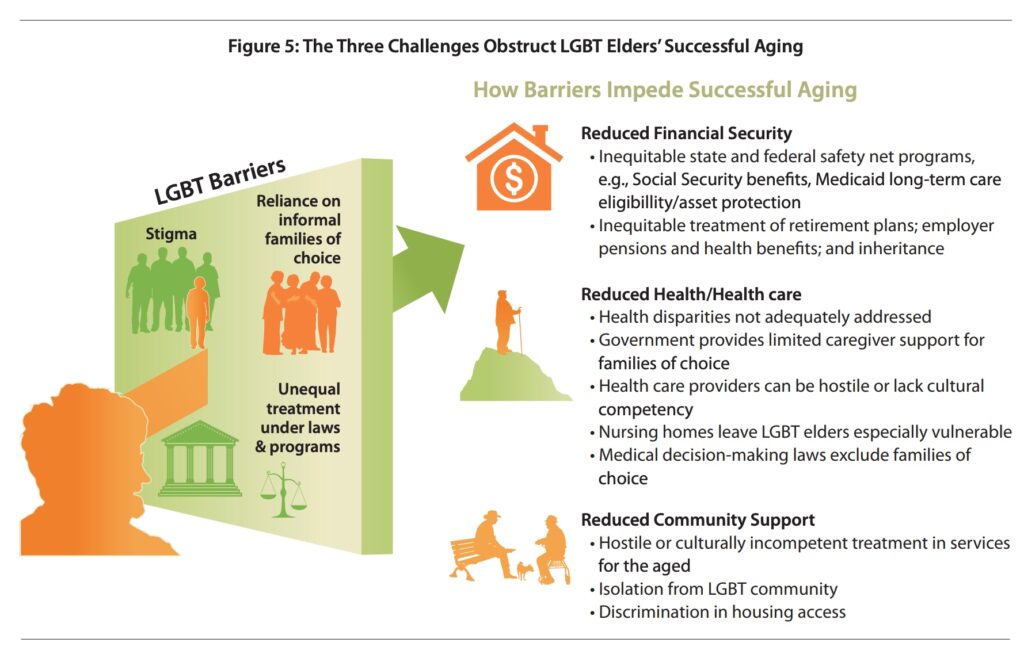
James Murray, 76, said he and his longtime partner faced another complication — they couldn’t afford to get married. “Tom would have lost his Medicaid and we might have lost our house,” Murray explained. “The rules for Medicaid are really stringent and if we had been married, he could have lost that access.”
Losing Medicaid would have been catastrophic for Murray’s partner, whose disability requires expensive medications and specialist appointments. “You have all these battles to fight and one of those is always where you fit in the system and how you can stay alive within it,” said Murray, a retired math teacher who has, with his partner of 32 years, lived in the same apartment for almost four decades.
“You don’t ever plan for catastrophe,” said Murray, whose partner was disabled in a car accident over a dozen years ago and then developed a heart condition. “But when catastrophe finds you, everything is just much harder day-to-day.”
Murray said that he has other friends who have had similar experiences of sudden devastating illness that has upended their lives. “My best friend’s partner had cancer and the treatments lasted over a year. It wiped out their savings and then he died. This is a common story and we are doing nothing about it. Absolutely nothing.”
SAGE (Services & Advocacy for GLBT Elders), the nation’s largest social service and advocacy group for LGBT elders, offers one study suggesting that they may be as much as five times less likely to access needed healthcare and social services. One study found that 75 percent of LGBT seniors interviewed reported not being open about their sexual orientation to healthcare workers for fear of discrimination. Both Cerise and Miller said they had faced discrimination with healthcare workers throughout the past few years of treatment. Miller changed doctors, Cerise could not.
LGBT baby boomers, the largest population of people 55 to 75, reported concern about discrimination as they age, with less than half saying they had confidence that healthcare professionals will treat them with dignity and respect, according to the study “Out and Aging: The MetLife Study of Lesbian and Gay Baby Boomers.” Fears of discriminatory treatment by healthcare professionals are particularly strong among lesbians, 12 percent of whom said they have no confidence that they would be treated respectfully.
In her practice as a therapist and clinical social worker, Dr. Jennie Goldenberg specializes in trauma. Outside her office door, a sign declares that it is a safe space for LGBTQ clients. “I want everyone to know, without having to ask, that they are welcome and can disclose their sexual orientation and gender identity in this space,” she said.
Goldenberg is acutely aware that such disclosure might not be easy and that LGBTQ people have issues with healthcare professionals that must be overcome. But, she explained, for LGBTQ elders, reaching out for therapy can be essential to survival.
“Social isolation is a major factor of depression in older adults,” she said. “LGBTQ elders have often experienced years of rejection from family members, friends and community — including faith communities. This has caused a pervasive sense of isolation.”
Reaching out is not easy, Goldenberg said. “LGBTQ elders don’t trust mental health professionals to have the cultural competence necessary to understand, nor the ability to empathize with their minority status within the larger culture.”
She added that LGBTQ elders “have experienced the cumulative effect of years of daily microaggressions. Lifetime experiences of discrimination and victimization based on sexual orientation have caused stigma, shame and the internalization of negative societal views of their sexual orientation and gender identity.”
For Miller, aging has become a battle in ways he never expected.
“I feel pretty good. I’d like to spend the next ten years with friends and traveling, and maybe being in another relationship. But the cost of this medication keeps me tied to working hours I don’t always feel able to work. And it’s made me depressed and resentful.”
There should be better services for LGBT elders, Miller says.
“We should be able to age the way we want to. Not the way we have to.”
Next week, a look at housing: where and how will LGBT people live as they age?