A research team led by investigators at Temple University and the University of Nebraska Medical Center have eliminated HIV from living animals for the first time, the scientists announced this month.
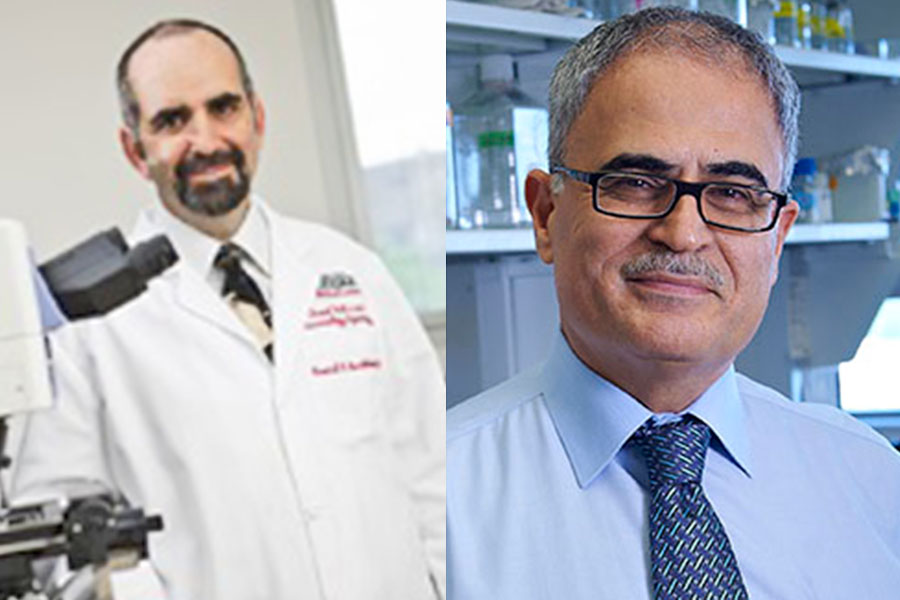
The study was published July 2 in the scientific journal “Nature Communications.” Since then, people from across the globe have reached out inquiring about a potential cure of HIV and AIDS, said Dr. Kamel Khalili, director of Temple’s Comprehensive NeuroAIDS Center and co-senior investigator on the research. Dr. Howard Gendelman, director of UNMC’s Center for Neurodegenerative Diseases and Philadelphia native, worked alongside him on the discovery.
In the experiment, Gendelman’s LASER ART technique, a slow-releasing strategy for targeting cells that commonly hold HIV, was followed by Khalili’s gene-editing CRISPR-Cas9 technology. The methods worked together better than existing antiretroviral therapy treatment to remove HIV, curing the disease in nine of 23 mice involved in the experiment.
“To my knowledge, this is the first time that scientists as a whole demonstrated that HIV can be cured,” Khalili told PGN.
Khalili and Gendelman, professionally acquainted for more than 25 years, have each devoted decades to fighting HIV.
Working in the medical field during the 1980s in the Bronx, New York City, Gendelman was on a team that saw some of the first patients with HIV during the early stages of the epidemic — a time he said made a “huge dent of grief.”
“It was many, many gay men who were coming in very young with diseases we hadn’t seen ever before, and it was devastating because we didn’t know what caused it,” Gendelman added. “We didn’t know why they had it, and we didn’t know what was happening.”
The first official report of the disease happened in 1981. Two years later, there were 3,064 AIDS cases in the United States — with a 42 percent morality rate. In 1992, the disease clocked in as the leading cause of death for U.S. men aged 25-44.
Today, more than half of those living with HIV across the world receive antiretroviral treatment to manage the virus. Preventative drugs like PrEP decrease chances of contracting the disease by up to 99 percent if taken daily. The Centers for Disease Control and Prevention estimate 1.1 million people in the United States now live with HIV, per 2016 data.
Khalili, a molecular biologist who earned his Ph.D. at the University of Pennsylvania, began researching a potential cure in the 1980s. So when the Temple-UNebraska team made its discovery after his more than 30 years of devotion, it was “unbelievable,” Khalili said.
But there’s still a road to an HIV cure.
The team now plans to advance from testing on mice to monkeys. Pending approval from the U.S. Food and Drug Administration, the scientists hope to begin clinical trials for humans by summer 2020, Khalili said. They are eying several clinics in the Philadelphia area to serve as the test site.
Khalili only wishes the process for finding a cure were quicker.
“I feel terrible that it’s not available right now,” he said. “But at least we know that it’s hopefully a new strategy to come up.”
To increase the cure rate in the study, Khalili said the team will tweak the method by calibrating the dosage and timing of his CRISPR technology. The crew has met once already with FDA representatives and will again before the end of the year to present final protocol strategies for the clinical trials.
The idea of a potential cure should still bring hope, Gendelman said. While drugs exist to manage HIV in a way not possible during the epidemic, people with HIV still experience stigma, co-occurring health conditions, neurological and cognitive impacts, stress in relationships and other issues, he said.
“The idea that new medicines are coming online that could potentially eliminate HIV forever in an easily-administered cocktail of drugs … has to make people smile in so many ways,” Gendelman added. n