Dr. Christine McGinn, a noted transgender surgeon in Bucks County, shared the story of a patient who had issues with two surgeries and underwent long-term therapy with her colleague Dr. Maureen Osborne.
“We need to talk about our complications,” McGinn told a room full of about 200 health professionals at Valley Forge Casino Resort. “We need to not get up here and say that every case works out great because it’s the person and their primary-care providers who will deal with this long-term.”
McGinn said urologists need to be aware of transgender care. She also noted some surgeons use a colon segment when constructing a neovagina, though it is not her preferred method, and doctors should be aware to scan the tissue for colon cancer and colitis.
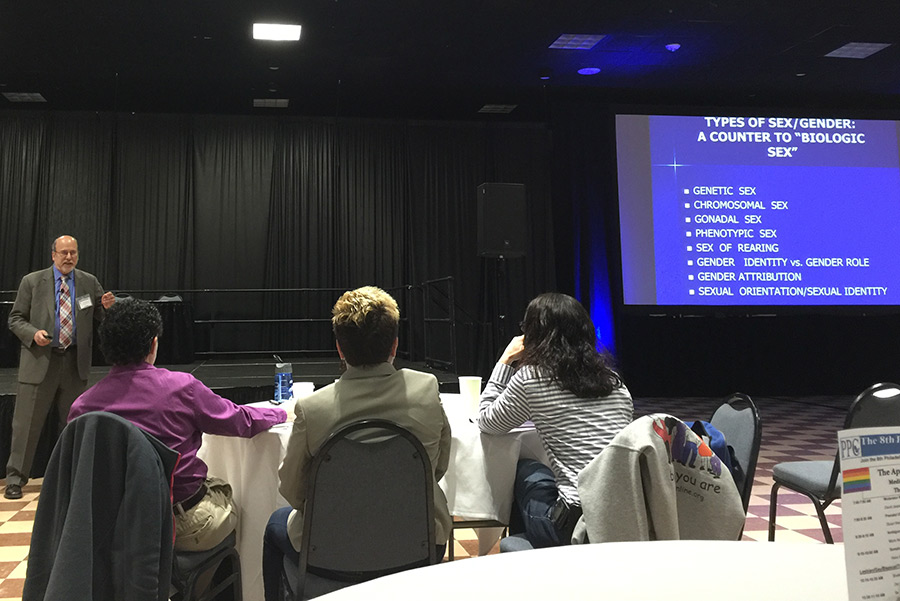
McGinn emphasized the importance of having a “gender team” so every person who provides health services to a patient understands the process and his or her role in it. She was speaking April 16 at the Transgender Medicine Symposium, hosted for the first time by the Philadelphia College of Osteopathic Medicine.
The audience included academics, medical students, primary-care providers, social workers, plastic surgeons, civil employment lawyers and insurance-company representatives. Fifteen health professionals spoke throughout the daylong event, including Dr. Kathy Rumer from Montgomery County and five others from Southeastern Pennsylvania.
“Some of the world’s top specialists in transgender care are in the Philadelphia area,” McGinn told PGN after her 90-minute discussion on procedures like vaginoplasty, phalloplasty and urethral lengthening. “Philadelphia’s always been a city that’s had this plethora of medical schools. But depending on the tide of insurance companies and what they’re willing to reimburse and the different protective laws for antidiscrimination, it does or does not create the right environment for that to flourish.”
McGinn added that in the last three to five years there has been an enormous surge of interest in transgender care from the medical community.
“There is access, but we’re a big state and in some places there is a problem with access,” Dr. Rachel Levine, Pennsylvania’s first transgender physician general, told PGN. She noted strong gender-care programs in Philadelphia and Pittsburgh as well as Dr. Jarrett Keller Sell from Penn State Hershey Medical Center and Alder Health Services in Harrisburg.
“Not every provider has to be able to provide gender-confirmation care,” Levine said. “But transgender individuals need primary care, they need specialty care and they need emergency care like anybody else. As more providers are accepting and welcoming to LGB and transgender patients, then patients will be more trusting and care will be better.”
Levine kicked off the Transgender Medicine Symposium with a discussion about transgender adolescents and their interactions with pediatric professionals. Some audience members said they were having trouble getting insurance coverage for estradiol, an estrogen hormone. Levine said any providers having this issue should email her at [email protected] and she would talk with the head of Medicaid about it.
Dr. Norman Spack, an endocrinologist and founder of Boston Children’s Hospital’s Gender Management Service, the first of its kind in the United States, also addressed hormone-replacement therapy.
Levine said providers could familiarize themselves with the accepted standards of care from the World Professional Association for Transgender Health by visiting wpath.org. Levine reminded providers that, when working with teens, it’s especially important to discuss what they envision for their reproductive futures to help them plan the best treatment. She also said young people should be prevented from smoking because it can cause blood clots during hormone therapy, and some physicians won’t prescribe hormones to patients who smoke.
Frances Conwell, a retired social worker from Wynnefield, was happy to attend the symposium. Since she started volunteering with Philadelphia FIGHT, a comprehensive AIDS-service organization, she said she started meeting a lot more transgender people.
“The country is changing,” she said. “I knew a little because I went to a couple trainings, but my awareness was not there even as a social worker. I worked with a lot of gay kids, but no trans kids. At least none who were out.”
Conwell said she wanted to learn how to better advocate for trans people. She also wanted to get more medical background information without putting a trans person on the spot about personal medical circumstances.
Dr. Lisa McBride, chief diversity officer and program co-chair at the Philadelphia College of Osteopathic Medicine, said the symposium was “definitely a success.”
“I’m happy with the amount of residents and student physicians there because I believe they’re the future of care,” McBride said.
She said the next steps for the college are to create a task force to improve continuity of care for transgender people and develop a center of excellence for transgender health. The University of California at San Francisco has a center, but McBride said there is nothing comparable on the East Coast.
“We need more evidence-based research” for transgender care, McBride said, “instead of consensus-based observations. We need to close the gap and have providers treat transgender patients as humans.”